Updates on Smoking & Low Back Pain
This review article highlights current knowledge on the association between low back pain and smoking, with an emphasis on the role of nicotine.
By Bilal F. Shanti, MD and Ihsan F. Shanti, MD, PhD
An estimated 1 in 5 adults in the United States uses tobacco products every day or some days. This equates to 50 million people and 21.3% of the overall population.1 Smoking is more common among men (26.2%) than women (15.4%) and is most common among adults aged 25 to 44 years (25.2%).1 Tobacco use remains the leading cause of preventable death in the United States, accounting for more than 480,000 deaths each year.2 In addition, more than 16 million Americans suffer from a smoking-related disease, including cancer, and respiratory and vascular diseases.2
Interestingly, the prevalence of tobacco use is nearly 2-fold higher among patients with chronic pain.3-5 The reasons for this increased prevalence are believed to be related to many factors, encompassing both behavioral and biological mechanisms. This review will cover current knowledge on the biological mechanisms and pathophysiology behind the relationship between smoking and chronic pain. The behavioral mechanisms are discussed in a Q&A with Joseph W. Ditre, PhD.
Cigarettes contain many compounds that produce physiologic effects, but this review focuses on nicotine, which is the most widely studied of these compounds and is believed to play a role in pain modulation. Nicotine has analgesic properties that, at first, can help relieve acute pain. However, over time, nicotine can alter pain processing and contribute to the development of chronic pain and greater pain intensity. This paradox is an important aspect of both acute and chronic pain management for patients who use tobacco products.
Mechanism of Nicotine Action
A variety of factors are believed to contribute to the analgesic effects of short-term exposure to nicotine.
First, nicotine is an agonist of nicotinic acetylcholine receptors (nAChRs), which are found throughout the peripheral and central nervous system, and notably in brain regions associated with pain transmission, such as the dorsal horn, locus ceruleus, and thalamus.6 Specifically, nicotine acts on the α3β4 ganglion type in the autonomic ganglia and adrenal medulla, and the α4β2 nicotinic receptors in the central nervous system.6,7 The increased binding of nAChRs produces central antinociceptive effects that activate the spinal cord descending pain-inhibitory pathways, resulting in discharge of epinephrine from the adrenal medulla and catecholamines from sympathetic nerve endings.8-10
Activation of nAChRs also potentiates the release of other neurotransmitters, such as dopamine, that play a role in nicotine-mediated analgesia.8,11 This increased stimulation of dopamine also activates the mesolimbic dopamine reward system, which increases the importance of incentive cues associated with nicotine use.6 Through this reward system, painful stimuli can become a conditioned cue for smoking.6 Interestingly, activation of nAChRs is similar to activation of opioid receptors in that both stimulate the release of dopamine in the nucleus accumbens, which mediates the rewarding effects of nicotine and plays a role in pain perception.8,12,13
Second, the antinociceptive effects of nicotine also may be mediated by activation of endogenous opioid systems.14,15 Smoking stimulates the release of beta-endorphins, which are endogenous opioid polypeptide compounds that are similar to opioids in their analgesic effects.16,17 The more cigarettes smoked per day, the higher the plasma concentration of beta-endorphins.6,18
Third, smoking causes changes in the neuroendocrine system that could modulate pain perception. In general, the stress response (sympathetic and hypothalamic-pituitary-adrenal [HPA] activation)7 causes a decrease in pain perception.8,19 However, this stress response is blunted in chronic smokers, possibly because of attenuated modulation of endogenous opioids on the HPA.19
Fourth, pressor actions on the cardiovascular system have been hypothesized to play a role in the analgesic effect of nicotine. Some studies suggest that passive smoking and smoking cigarettes increases blood pressure, which in turn has been linked to reduced pain sensitivity.6,20-23
Other proposed mechanisms for the analgesic effects of nicotine include attentional narrowing, release of norepinephrine and serotonin, g-aminobutyric acid (GABA) receptor activity, regulation of inflammatory responses, and suppression of pain-related evoked potentials.6,24-28
While all of these analgesic effects of nicotine occur with brief exposure to nicotine, chronic nicotine exposure is linked to nAChR desensitization and tolerance29-31 and changes in the endogenous opioid system that may alter pain processing.31
Smoking and Chronic Pain Studies
It is important to differentiate the effects of nicotine in experimental versus epidemiologic studies. While experimental studies suggest an analgesic and antinociceptive effect of tobacco use in acute pain, epidemiologic studies point to a causal association between smoking and chronic pain.
Experimental Studies
Experimental studies point to analgesic and antinociceptive effects in acute pain. For example, in early research by Tripathi et al, the researchers assessed the analgesic effect of nicotine by measuring tail-flick latency in rats and mice.32 Brain levels of nicotine reached a maximum at 10 minutes, whereas antinociception was maximal at 2 minutes. Tachyphylaxis to antinociception developed in 10 minutes and lasted up to 14 hours. In a 1998 study, Jamner et al found that nicotine increased pain threshold and tolerance ratings of men but had no effect on pain ratings of women.33 In 2004, Flood et al studied the effects of intranasal nicotine for postoperative pain treatment. They found that patients treated with nicotine reported lower pain scores during the first hour after surgery and less pain 24 hours after surgery, and used half the amount of morphine as the control group.34
While short-term exposure to nicotine appears to have antinociceptive effects, chronic exposure to nicotine may change pain perception due to receptor desensitization. Indeed, studies suggest that nicotine withdrawal increases pain sensitivity and blunts stress response in chronic smokers in experimental pain tests, and that this effect drives excessive nicotine use via corticotropin-releasing factor signaling pathways.35,36
Epidemiologic Studies
While an early landmark meta-analysis by Leboeuf-Yde did not show a consistent statistically significant positive association between smoking and low back pain (LBP) in studies published between 1974 and 1996,37 a resurgence of interest in this issue has produced more research in this field. Numerous recent studies have demonstrated an association between smoking and the prevalence of a variety of chronic pain conditions.38-41 In addition, chronic pain patients who smoke have greater pain intensity than those who do not smoke.42
In a study involving 10,916 patients, Ekholm et al found that cigarette smoking was significantly increased in individuals suffering from chronic pain; in opioid users, smoking was further increased.5 In addition, in a well-organized survey involving 73,507 people (aged 20-59 years), Alkherayf et al found a higher prevalence of LBP in daily smokers compared with nonsmokers (23.3% vs 15.7%; P<0.0001).43 This association was statistically significant in all age groups and genders, and was strongest in younger age groups. The data suggested a positive correlation between the smoking dose and the risk for LBP.
Further evidence of the link between smoking and pain chronicity is found in a study of 6,092 women over the age of 18 years reported by Mitchell et al.44 Women who smoked daily had a 2-fold higher prevalence of chronic pain compared with women who never smoked. In addition, women who were “some-day” smokers had a 1.8-fold increased prevalence of chronic pain.
Smoking was linked to an increased risk for transitioning from subacute back pain to chronic back pain in a 2014 study by Petre et al. Brain imaging in the study participants suggested that the risk for development of chronic back pain was linked to corticostriatal circuitry involved in addictive behavior and motivated learning in the nucleus accumbens and medial prefrontal cortex.45
While the etiology of chronic pain is multifactorial, these data suggest that smoking is a risk factor for development of chronic pain.
Nicotine-Induced Structural Changes Might Contribute to Chronic Pain Conditions
In addition to altering pain processing, smoking can contribute to structural changes that may increase the risk for chronic pain conditions. For example, smokers are at increased risk for osteoporosis, fracture, lumbar disc disease, impaired wound healing, muscular damage, and impaired healing from spinal fusion, possibly because of impaired oxygen delivery to tissues and accelerated degenerative processes.8,46-56
Conclusion
Although clinicians barely have time to finish their medical records, this should not preclude them from talking to their pain patients about smoking cessation. We must dedicate time to this task, provide our patients with educational materials, and keep the door open to bring up the subject on subsequent follow-ups. In a well-designed cohort study, Kaye et al showed that persistence on the part of the physician can significantly reduce both the amount and prevalence of nicotine consumption among pain patients in a relatively short amount of time.57 Given the impact of smoking on pain chronicity, it is imperative that physicians implement strategies to help their patients stop smoking.
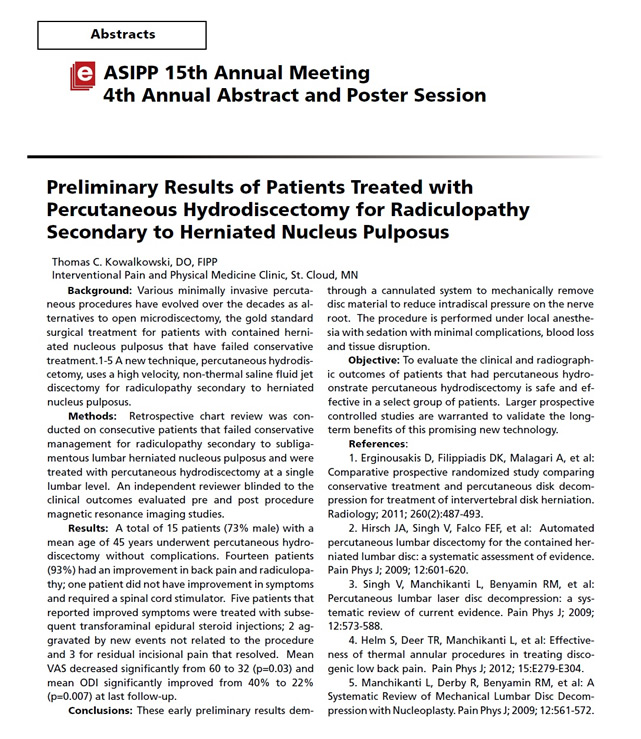
Dr. Thomas Kowalkowski, Medical Director of IPPMC, Intervention Pain and Physical Medicine Clinic, recently was selected to present his research findings, at the Annual Scientific Research meeting in Orlando, Florida. His presentation title was The results of Patients treated with Percutaneous Hydrodiscectomy for Radiculopathy Secondary to Herniated Nucleus Pulposis. The International Spine Interventional Society (ISIS), is an organization of over 3,000 physicians dedicated to the development and promotion for the highest standards of practice of interventional procedures in the diagnosis and treatment of spine pain.
"Water Jet" treatment at Sartell Clinic offers chance to wash away that disc pain

Photo by: Jason Wachter
Dr. Thomas Kowalkowski, medical director of the Interventional Pain and Physical Medicine Clinic in Sartell, shows a new device called HydroCision Sept. 17. The device is a minimally invasive treatment that uses high-speed water to remove herniated disc tissue without invasive surgery.
Who is a good candidate for HydroCision?
- Those with a bulging spinal disc that has not ruptured into the spinal canal.
- Someone whose pain has not improved after four or more weeks of conservative care, which typically consists of physical therapy, pain medications, and if necessary, epidural steroid injections.
- A person with signs of nerve damage in the leg (severe weakness, loss of coordination, loss of feeling).
Source: HydroCision Inc.
After undergoing HydroCision for herniated discs
- In most cases, you will be able to go home the same day as your procedure.
- Plan on bed rest with gentle stretching for several days.
- You may need over-the-counter or prescription pain medication for several days.
Source: HydroCision Inc.
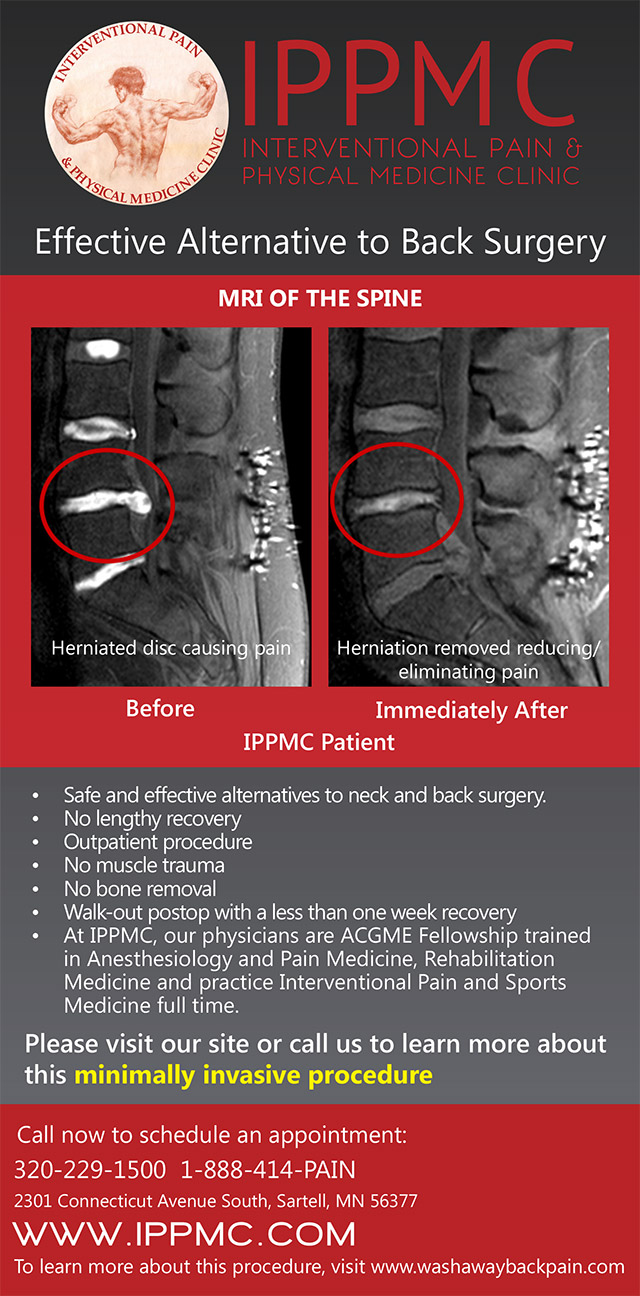
What if you could “wash away” back and leg pain using a “blade” that never gets dull?
A powerful water jet cutting device can be used for minimally invasive treatment of herniated discs, and Dr. Thomas Kowalkowski is the only physician in Central Minnesota to offer the procedure. “It’s basically a high-velocity water jet eroding system,” Kevin Staid said about the medical device that his North Billerica, Mass.-based company makes. “And this is our first entry into the area.”
With HydroCision, a jet of saline solution comes out of a nozzle that is 0.005 inches in diameter — “slightly larger than a hair” — and can cut away protruding disc tissue that can cause the back and leg pain without an actual blade.
“Just the energy of the jet would be doing the cutting,” said Staid, an engineer. “In our case, the water is going about 600 miles an hour and has the ability to cut quite effectively.”
The advantages of the 20-minute outpatient procedure are: No hospitalization, quicker recovery times, less pain, no surgical trauma to the back muscles and no general anesthesia. “There is no muscle damage, no bone removal, no nerve root manipulation ... and the size of the wound is approximately 4 mm,” Kowalkowski said.
Kowalkowski began offering HydroCision a few years ago to his patients; he is the medical director of the Interventional Pain and Physical Medicine Clinic in Sartell.
“The procedure and the study I have completed on it was published in a pain journal this summer,” he said of the official publication of the International Association for the Study of Pain.
HydroCision
Water-based tools previously have been used outside the medical field. “They were used in the aerospace industry and automotive industry for cutting and preparing things ... because the blade never gets dull or gunky,” Staid said.
HydroCision Inc. brought its cutting device into the medical field in 2005, and disc treatment is one of the uses.
When the outer wall of a spinal disc becomes damaged or weakened through age or injury, the inner part of the disc may bulge out in what is known as “disc herniation” or a “slipped” disc.
The water jet comes out of a tiny tube at the end of a spark plug-like tip and is collected — along with the blasted tissue — in another tube built into the same probe, completing a circuit of sorts.
“When the physician’s foot is not on the control pedal, it’s nothing but a benign metal probe,” said Staid, who came up with the concept with Tim Moutafis, a colleague.
Staid is the chief technology officer and vice president of application development at HydroCision Inc., a developer and manufacturer of fluidjet-based surgical tools.
“He (Moutafis) came upon the idea of using high-velocity water jets as a tool, which had been used extensively in industry but not had been developed for use in medicine at all,” Staid said. Kowalkowski said, “I really became intrigued with the technology, to a point that we’ve performed probably over 50 procedures, and many of those patients have been offered surgery as an option for their disc herniation.”
Spinal discs
Only spinal discs that have not ruptured may be treated with the water-based procedure, according to Kowalkowski.
HydroCision costs about $2,000 to perform at his Sartell clinic and may be covered by insurance — compared with the estimated $15,000 it would cost for surgery, he said.
“There is a week’s recovery time versus, many times, eight weeks or more with surgery,” Kowalkowski said. He also said that in the worst-case scenario that HydroCision does not work, the patient could still have surgery; HydroCision has between a 73 and 98 percent success rate. The physician uses a fluoroscope, which is a machine that projects live X-ray images onto a monitor, to place the water-dispensing probe within the disc.
“The patient is not even fully anesthetized. They’re awake and alert on the table,” Staid said. The system has been used in more than 45,000 spinal, arthroscopic and wound debridement procedures, according to HydroCision Inc.
“We’ve been able to document a physiological reduction in the size of the disc immediately after the procedure,” Kowalkowski said
Harnessing physics
Most people in the United States will experience lower back pain at least once during their lives, and more severe leg pain can affect one’s ability to walk, according to the Mayo Clinic.
“At the end of the day, it was hard to even walk because I just ached so bad, and I couldn’t do the activities that I used to be able to do,” said Amy Rasmussen, a patient of Kowalkowski’s.
The 36-year-old registered nurse from Zimmerman said based on her work in a health care setting, she believes not a lot of physicians are aware of HydroCision Inc.
“I work in patient care, and I was lifting a patient and that kind of ruined my back,” Rasmussen said. Her injury occurred when she was working with a 350-pound patient.
She said she has experienced lower back pain, swelling, and achy hips and legs because of the injury and had a lot of frustration before she tried HydroCision in August.
“I figured it was worth it to try this procedure because when you are in that much pain, you’re willing to do anything, and the minute the procedure was done, that pain was gone immediately,” she said.
Source: Stcloudtimes.com
FDA Warns of Serious Rash Risk with Acetaminophen Pills
Source: NBCnews.com
Tylenol and other painkillers containing the ingredient acetaminophen can cause potentially deadly rashes and blistering of the skin, U.S. health regulators warned on Thursday.
Companies that sell prescription acetaminophen will be required to add a warning about the risk of rash to the prescribing information, the Food and Drug Administration said.
Two of the skin conditions, Stevens-Johnson Syndrome and toxic epidermal necrolysis, can be fatal. They typically begin with flu-like symptoms, followed by rash, blistering, and the detachment of the upper surface of the skin, the FDA said.
A separate condition, acute generalized exanthematous pustulosis, is typically not life-threatening and is characterized by the sudden appearance of red skin containing dozens or hundreds of small blisters filled with white or yellow fluid.
The warning is based on new information gleaned from the FDA's data base of reported adverse events and medical literature. The agency said it is difficult to determine how frequently such skin reactions occur due to the widespread use of the drug, but it is likely the events occur rarely.
Other drugs used to treat fever and pain such as ibuprofen and naproxen also carry the risk of serious skin conditions, but the risk is already described in the warning section of those drug labels, the FDA said.
The agency will also request or encourage companies who sell acetaminophen products over the counter to add warnings about the rash risk.
New, Moving or Expanding: IPPMC Welcomes MRI Machine
Practice recently earned excellence award
Source: Stcloudtimes.com

SARTELL — A 5,000-square-foot expansion is nearing completion at the Interventional Pain & Physical Medicine Clinic (IPPMC). One of the latest pieces to fall in place was a new 12,000-pound MRI machine workers moved into place Monday with a forklift.
IPPMC started in 2003 in a small building on Stearns Way. Five years later, it moved to a 15,000-square-foot building at 2301 Connecticut Ave. The additional 5,000 feet was necessary to accommodate more patients and staff, according to Dr. Thomas Kowalkowski, who founded the practice.
For three years, the clinic had been using an MRI machine in a semi trailer parked outside the front door.
“This is a newer machine, and it’s going to be a permanent part of our facility, so we can continue to provide people the best care possible,” said Kowalkowski, who graduated from St. John’s University, the University of New England and completed a fellowship in anesthesiology and pain medicine at Oregon Health and Science University.
IPPMC has about 50 employees, and its building now features everything from an organic coffee and juice bar to a whirlpool, exercise pool and sauna, to a fully-stocked gym. The clinic also has openings for nine more full- and part-time positions.
“I wanted to come back here because this is home to me,” Kowalkowski said. “We’re the only multidisciplinary pain program of this level outside the Twin Cities, and people are responding to that.”
Earlier this month, IPPMC earned the Excellence in Pain Practice Award from the World Institute of Pain.
IPPMC is one of 17 pain centers in 11 countries to receive the honor.
WIP announces Excellence in Pain Practice Award recipient
WINSTON-SALEM, North Carolina, USA (March 11, 2013) – The World Institute of Pain (WIP) has conferred the Excellence in Pain Practice (EPP) Award for Multidisciplinary Clinical Pain Practice on the Interventional Pain and Physical Medicine Clinic (IPPMC) in Sartell, Minnesota, USA.
“IPPMC’s attributes include providing a multidisciplinary pain centered approach to the prevention, evaluation, treatment, and rehabilitation of painful disorders,” said Dr. Bruce Wymore, a family practitioner in Alexandria, Minnesota.
Dr. Jose Veliz, a pain medicine specialist in Escondido, California added that IPPMC Medical Director Dr. Thomas Kowalkowski has, “a true passion for pain medicine. “
In conveying the award, WIP’s EPP Award Committee Chairman, Dr. P. Prithvi Raj said, “The Committee found the Interventional Pain and Physical Medicine Clinic’s multidisciplinary approach to clinical pain practice to be exemplary. The impact of this pain center on the specialty of pain practice is evident through its individualized approach to improving the quality of life by reducing pain and suffering, through teamwork and a multi-disciplinary model of care.”
The EPP Award program, established in 2010 by the World Institute of Pain, recognizes pain centers that demonstrate the highest standards of pain practice around the world. Varying levels of recognition are attainable, including specialization in a particular area of clinical pain practice, multidisciplinary clinical pain practice, and comprehensive recognition that encompasses all dimensions of pain management including cutting-edge research. EPP Awards have been conferred on 17 pain centers in 11 countries.
To qualify for the award, a site visit is conducted by an FIPP (Fellow of Interventional Pain Practice) member of WIP’s inspector’s panel. The EPP Award Committee exercises its due diligence in the determination of each award given, in accordance with WIP’s guidelines for EPP Award recognition.
WIP is an international, nonprofit organization founded in 1993 that brings together the most recognized experts in the field of pain medicine for the advancement and standardization of interventional pain practice. WIP achieves its purposes and objectives through organizing physician-oriented educational symposia, practical workshops, and World Congresses; certifying as Fellows of Interventional Pain Practice (FIPP) physicians who pass a competency-based, multi-part examination; publishing the scholarly journal, Pain Practice; and establishing liaisons with physicians and industry worldwide to promote the specialty of pain medicine.
IPPMC Patients need NOT be concerned with the multi-state meningitis and septic arthritis outbreak. IPPMC has not utilized these pharmaceutical products. All medications at IPPMC are FDA Approved. IPPMC is dedicated to offering the highest standard of care based on patient outcomes.