Kristoff Kowalkowski is selected among the nation’s best
Standout Kristoff Kowalkowski is Among America’s Top Prep Football Athletes to Gather at Football University Top Gun Showcase in Dublin, Ohio.
St. Cloud, MN (7/7/15) – Kristoff Kowalkowski of St. John’s Prep, from (St. Cloud, Mn) has been invited and will be competing at the nation’s top prep football all-star camp, Football University (FBU) Top Gun, at Dublin Jerome High School in Dublin, Ohio from Monday, July 20 to Wednesday, July 22. Being a part of FBU Top Gun means that these players are considered the best at their respective positions.
Kristoff Kowalkowski, was invited to Top Gun because of his outstanding performance as a QB at the FBU Minneapolis camp. He will join more than 1,600 of the nation’s top athletes at their respective positions and will train with current and former NFL coaches and players.
Top Gun is the culmination of Football University’s 24-camp nationwide camp season gathering the most elite performers from across the United States and allowing them to compete and display their abilities together on one stage. Football University has an impressive alumni list that includes some of the top college football recruits and players in the nation. Headlining the Top Gun Showcase coaching staff are quarterbacks coach Jeff Rutledge, former quarterback coach of the Arizona Cardinals; running back coach Robert Edwards, offensive line coach Jim McNally, who is considered the best offensive line coach in the game; defensive back coach Ray Buchanan; and wide receiver coach Charlie Collins, who is considered one of the finest receiver coaches in the game.
247Sports on Football University Top Gun: “No event is bigger than Football University Top Gun. It is easily the most highly-anticipated camp for us because of the level of talent.”
6 Reasons To Drink Green Tea... Starting Today
Source: MSH Health
The green miracle drink from China made its way long ago into the mugs of Americans all across the nation for its touted health benefits. From a weight loss aid to targeting pancreatic cancer, green tea has evolved into a medicinal drink that caters to a myriad of illnesses. The reality is there are surprising benefits to reap from this magical drink in just one cup.
The hot beverage accounts for 15 percent of the tea consumed in the U.S., according to the Tea Association’s latest statistics. Although black tea remains America’s favorite at 84 percent, green tea can invite more positive changes when it comes to your health. Unlike green tea, black tea is processed in a way that allows for fermentation, which depletes the amount of antioxidants and polyphenols found in tea. Black tea also contains less catechins than green tea, which minimizes the benefits of the hot beverage
Here are surprising health reasons why you should go green and let it be your cup of tea:
1. Combats Allergies
Green tea may need to be added to your allergy season arsenal. Drinking the green liquid may provide some relief, as it's been proven to be anti-allergenic; a specific compound, epigallocatechin gallate (EGCG), appears to be the most potent.
A 2007 study published in the journal Cytotechnology found the tea polyphenol can reduce pollen allergies. This is the first time a methylated form of EGCG can block the IgE receptor — the key receptor involved in an allergic response. It can elicit a stronger anti-allergenic response than normal EGCG, which makes it the strongest anti-allergen compound found in tea. Quercetin, a naturally occurring flavonol in tea, can also alleviate a histamine response.
2. Boosts Eyesight
Carrots have long been associated as a food that promotes good eyesight, but science suggest there’s a new kid on the block. The antioxidants found in green tea can actually penetrate the tissues of the eyes and produce antioxidant activity. Catechins, an antioxidant in green tea, are capable of being absorbed into the tissues of the eye.
A 2001 study published in the journal Experimental Eye Research found green tea can actually prevent cataract-induced blindness. Researchers saw different parts of the eye absorbed varying amounts of catechins, with the highest concentration of this antioxidant found in the retina of lab rats fed green tea extract. The area with the least absorption of catechins was the cornea. These findings suggest that drinking green tea could serve as a protective measure when it comes to eyesight, but its effects have yet to be confirmed in humans.
3. Lowers Cholesterol
The access to greasy foods puts your health at risk for heart-related complications like high cholesterol. Replacing unhealthy snacks and drinks with green tea could actually help keep your cholesterol levels at bay. Green tea’s powerful antioxidant, EGCG, is believed to inhibit the absorption of cholesterol from the large intestine.
A 2011 study published in The American Journal of Clinical Nutrition found green tea consumption significantly lowered the total serum cholesterol and LDL cholesterol across 14 randomized controlled trials of over 1100 participants. Overall, green tea intake led to significant reductions in total cholesterol — 7.2mg/dL, and mean low-density lipoprotein (LDL) cholesterol (2.19 mg/dL). Research suggests drinking five cups of green tea per day will provide the biggest reduction in cholesterol.
4. Promotes Healthy Gums And Teeth
Drinking tea has been given a bad reputation for its staining effect on your teeth. The hot beverage contains tannic acid, which is what gives tea its dark-like color. However, the consumption of green tea can actually be beneficial when it comes to your oral health.
A 2009 study published in the Journal of Periodontology found the intake of green tea was inversely correlated with periodontal disease. Regularly drinking green tea reduced symptoms of periodontal disease, possibly due to the presence of catechin. Catechin reduces inflammation in the body, and therefore, interferes with the body’s inflammatory response to periodontal bacteria. Its ability to control bacteria and lower the acidity of saliva and dental plaque makes it useful for preventing cavities and other indicators of poor oral health.
5. Wards Off Oral Cancer
Green tea has been known to target pancreatic cancer, and most recently oral cancer. Its strongest antioxidant, EGCG, is able to help kill cancer cells through destruction of the cells’ mitochondria, and may even become a possible alternative to the debilitating chemotherapy. Green tea consumption is believed to not be associated with any of chemo’s side effects, according to a recent study published in the journal Molecular Nutrition & Food Research.
“It looks like EGCG causes the formation of reactive oxygen species in cancer cells, which damages the mitochondria, and the mitochondria responds by making more reactive oxygen species,” Joshua Lambert, associate professor of food science at Penn State, in a press release. Eventually, the mitochondria loses its defenses with a breakdown in the expression of antioxidant genes. It is in this weakened state the cancer cells succumb to EGCG and die.
6. UV Protection
You may want to add a packet of green tea in addition to sunscreen and sunglasses when you visit the beach. The catechins in green tea can actually make the skin more resistant to the effects of UV rays and therefore premature skin aging. They can also lead to reduced skin redness after UV exposure.
A 2013 study published in the British Journal of Nutrition found a relatively low dose (540 mg) of green tea catechins each day along with 50 mg of vitamin C for 12 weeks, or two cups of green tea can considerably reduce the effect of UV radiation on the skin. When UV exposure produced inflammation, green tea supplementation reduced that effect. This is the first time oral doses of green tea has been proven to make their way to skin tissues to limit the effects of the sun’s ultraviolet rays.
A cup of green tea a day, may actually keep the doctor away
Kill your sugar addiction with these 5 simple steps
Source: MSH Health
As scientists continue to study and learn more about its effects, we’re continuing to learn why sugar should be only a very small part of diets.Among other health issues, in excess, sugary foods and beverages like soda, candy and even snack bars and cereals contribute to weight gain and obesity, impaired memory, and an increased risk for heart disease and diabetes.
Plus, as Rene Ficek, a registered dietitian and the lead nutrition expert at Seattle Sutton's Healthy Eating points out, “For many of us, indulging in these foods has created an insatiable sweet tooth.”Essentially, the more you eat sugar, the more you’re likely to continue craving it.“But we must work on controlling sugar cravings,” Ficek said. “By getting sugar cravings under control you will have a better chance to maintain your healthy eating habits in the long run.”
First and foremost, Ficek does not recommend trying to “kill your addiction” through a cold turkey detox or any other similar method.“If you believe you eat too much sugar, why not try cutting back rather than abstaining 100 percent?,” Ficek said. “Forcing yourself to eliminate sugar completely for any length of time increases the likelihood of binging on it at some point.” For this reason, Ficek says, instead it’s important to find a balance in your diet and practice moderation.“The all-or-nothing approach when it comes to food often fails and sets dieters up for a harmful yo-yo diet cycle,” she added. Ficek also notes that you should recognize the difference between added sugar (like table sugar and concentrated sources like in fruit juice) and naturally occurring sugars (like those found in fruits, vegetables, full fat dairy, honey and unrefined carbohydrates).
“These naturally occurring sugars are valid energy sources, and along with the other nutrients in these foods, are important for nourishing a healthy body,” she said. “While eliminating added sugars from the diet is possible—but may be very difficult to do—eliminating all sugars from the diet may end up being harmful to one’s health. So, start with these simple tips to eliminate the excess, added sugar from your diet.”
1. Read Labels
Ficek says: Begin your sugar “detox” by avoiding adding sugar to your drinks and meals, and curb obviously sweet foods like candy bars, pastries and sodas. Start reading labels on the items in your refrigerator and pantry. Many foods like sauces, condiments, soups and of course sodas have added sugar. It may masquerade under a different name, but rest assured that any ingredient that ends in “-ose” probably means sugar. This process will likely be quite daunting; as most packaged, canned and otherwise processed and preserved foods have added sugar.
2. Drink Water
Ficek says: When your body is dehydrated it actually craves sweets, so by drinking a lot of water during the day you can decrease your sugar cravings and give your body more energy. When you are first starting out, drink at least one large glass of water each hour of the work day.
3. Jumpstart your Health With Whole Foods
Ficek says: If you know that you are addicted to sugar and experience headaches and body aches after not having sweets, it is even more important to jumpstart your health by eating real whole foods to help cleanse your body from toxins and give you more energy.
4. Increase Your Greens
Ficek says: Adding greens to your diet is one of the best ways to keep energy levels up and eliminate those sweet cravings. Try having a green smoothie for breakfast, a big salad for lunch and a green veggie stir fry for dinner. These meals will make you feel so good; you won’t dare go back to those sweet treats.
5. Satisfy Sweet Cravings with Fruit
Ficek says: When craving chocolate or cookies, why not try an apple instead? You may be surprised with how satisfied you feel after. The natural sugars and fiber in whole fruits will provide the sweetness you are craving without the blood sugar spike, keeping energy and moods lifted.
Updates on Smoking & Low Back Pain
This review article highlights current knowledge on the association between low back pain and smoking, with an emphasis on the role of nicotine.
By Bilal F. Shanti, MD and Ihsan F. Shanti, MD, PhD
An estimated 1 in 5 adults in the United States uses tobacco products every day or some days. This equates to 50 million people and 21.3% of the overall population.1 Smoking is more common among men (26.2%) than women (15.4%) and is most common among adults aged 25 to 44 years (25.2%).1 Tobacco use remains the leading cause of preventable death in the United States, accounting for more than 480,000 deaths each year.2 In addition, more than 16 million Americans suffer from a smoking-related disease, including cancer, and respiratory and vascular diseases.2
Interestingly, the prevalence of tobacco use is nearly 2-fold higher among patients with chronic pain.3-5 The reasons for this increased prevalence are believed to be related to many factors, encompassing both behavioral and biological mechanisms. This review will cover current knowledge on the biological mechanisms and pathophysiology behind the relationship between smoking and chronic pain. The behavioral mechanisms are discussed in a Q&A with Joseph W. Ditre, PhD.
Cigarettes contain many compounds that produce physiologic effects, but this review focuses on nicotine, which is the most widely studied of these compounds and is believed to play a role in pain modulation. Nicotine has analgesic properties that, at first, can help relieve acute pain. However, over time, nicotine can alter pain processing and contribute to the development of chronic pain and greater pain intensity. This paradox is an important aspect of both acute and chronic pain management for patients who use tobacco products.
Mechanism of Nicotine Action
A variety of factors are believed to contribute to the analgesic effects of short-term exposure to nicotine.
First, nicotine is an agonist of nicotinic acetylcholine receptors (nAChRs), which are found throughout the peripheral and central nervous system, and notably in brain regions associated with pain transmission, such as the dorsal horn, locus ceruleus, and thalamus.6 Specifically, nicotine acts on the α3β4 ganglion type in the autonomic ganglia and adrenal medulla, and the α4β2 nicotinic receptors in the central nervous system.6,7 The increased binding of nAChRs produces central antinociceptive effects that activate the spinal cord descending pain-inhibitory pathways, resulting in discharge of epinephrine from the adrenal medulla and catecholamines from sympathetic nerve endings.8-10
Activation of nAChRs also potentiates the release of other neurotransmitters, such as dopamine, that play a role in nicotine-mediated analgesia.8,11 This increased stimulation of dopamine also activates the mesolimbic dopamine reward system, which increases the importance of incentive cues associated with nicotine use.6 Through this reward system, painful stimuli can become a conditioned cue for smoking.6 Interestingly, activation of nAChRs is similar to activation of opioid receptors in that both stimulate the release of dopamine in the nucleus accumbens, which mediates the rewarding effects of nicotine and plays a role in pain perception.8,12,13
Second, the antinociceptive effects of nicotine also may be mediated by activation of endogenous opioid systems.14,15 Smoking stimulates the release of beta-endorphins, which are endogenous opioid polypeptide compounds that are similar to opioids in their analgesic effects.16,17 The more cigarettes smoked per day, the higher the plasma concentration of beta-endorphins.6,18
Third, smoking causes changes in the neuroendocrine system that could modulate pain perception. In general, the stress response (sympathetic and hypothalamic-pituitary-adrenal [HPA] activation)7 causes a decrease in pain perception.8,19 However, this stress response is blunted in chronic smokers, possibly because of attenuated modulation of endogenous opioids on the HPA.19
Fourth, pressor actions on the cardiovascular system have been hypothesized to play a role in the analgesic effect of nicotine. Some studies suggest that passive smoking and smoking cigarettes increases blood pressure, which in turn has been linked to reduced pain sensitivity.6,20-23
Other proposed mechanisms for the analgesic effects of nicotine include attentional narrowing, release of norepinephrine and serotonin, g-aminobutyric acid (GABA) receptor activity, regulation of inflammatory responses, and suppression of pain-related evoked potentials.6,24-28
While all of these analgesic effects of nicotine occur with brief exposure to nicotine, chronic nicotine exposure is linked to nAChR desensitization and tolerance29-31 and changes in the endogenous opioid system that may alter pain processing.31
Smoking and Chronic Pain Studies
It is important to differentiate the effects of nicotine in experimental versus epidemiologic studies. While experimental studies suggest an analgesic and antinociceptive effect of tobacco use in acute pain, epidemiologic studies point to a causal association between smoking and chronic pain.
Experimental Studies
Experimental studies point to analgesic and antinociceptive effects in acute pain. For example, in early research by Tripathi et al, the researchers assessed the analgesic effect of nicotine by measuring tail-flick latency in rats and mice.32 Brain levels of nicotine reached a maximum at 10 minutes, whereas antinociception was maximal at 2 minutes. Tachyphylaxis to antinociception developed in 10 minutes and lasted up to 14 hours. In a 1998 study, Jamner et al found that nicotine increased pain threshold and tolerance ratings of men but had no effect on pain ratings of women.33 In 2004, Flood et al studied the effects of intranasal nicotine for postoperative pain treatment. They found that patients treated with nicotine reported lower pain scores during the first hour after surgery and less pain 24 hours after surgery, and used half the amount of morphine as the control group.34
While short-term exposure to nicotine appears to have antinociceptive effects, chronic exposure to nicotine may change pain perception due to receptor desensitization. Indeed, studies suggest that nicotine withdrawal increases pain sensitivity and blunts stress response in chronic smokers in experimental pain tests, and that this effect drives excessive nicotine use via corticotropin-releasing factor signaling pathways.35,36
Epidemiologic Studies
While an early landmark meta-analysis by Leboeuf-Yde did not show a consistent statistically significant positive association between smoking and low back pain (LBP) in studies published between 1974 and 1996,37 a resurgence of interest in this issue has produced more research in this field. Numerous recent studies have demonstrated an association between smoking and the prevalence of a variety of chronic pain conditions.38-41 In addition, chronic pain patients who smoke have greater pain intensity than those who do not smoke.42
In a study involving 10,916 patients, Ekholm et al found that cigarette smoking was significantly increased in individuals suffering from chronic pain; in opioid users, smoking was further increased.5 In addition, in a well-organized survey involving 73,507 people (aged 20-59 years), Alkherayf et al found a higher prevalence of LBP in daily smokers compared with nonsmokers (23.3% vs 15.7%; P<0.0001).43 This association was statistically significant in all age groups and genders, and was strongest in younger age groups. The data suggested a positive correlation between the smoking dose and the risk for LBP.
Further evidence of the link between smoking and pain chronicity is found in a study of 6,092 women over the age of 18 years reported by Mitchell et al.44 Women who smoked daily had a 2-fold higher prevalence of chronic pain compared with women who never smoked. In addition, women who were “some-day” smokers had a 1.8-fold increased prevalence of chronic pain.
Smoking was linked to an increased risk for transitioning from subacute back pain to chronic back pain in a 2014 study by Petre et al. Brain imaging in the study participants suggested that the risk for development of chronic back pain was linked to corticostriatal circuitry involved in addictive behavior and motivated learning in the nucleus accumbens and medial prefrontal cortex.45
While the etiology of chronic pain is multifactorial, these data suggest that smoking is a risk factor for development of chronic pain.
Nicotine-Induced Structural Changes Might Contribute to Chronic Pain Conditions
In addition to altering pain processing, smoking can contribute to structural changes that may increase the risk for chronic pain conditions. For example, smokers are at increased risk for osteoporosis, fracture, lumbar disc disease, impaired wound healing, muscular damage, and impaired healing from spinal fusion, possibly because of impaired oxygen delivery to tissues and accelerated degenerative processes.8,46-56
Conclusion
Although clinicians barely have time to finish their medical records, this should not preclude them from talking to their pain patients about smoking cessation. We must dedicate time to this task, provide our patients with educational materials, and keep the door open to bring up the subject on subsequent follow-ups. In a well-designed cohort study, Kaye et al showed that persistence on the part of the physician can significantly reduce both the amount and prevalence of nicotine consumption among pain patients in a relatively short amount of time.57 Given the impact of smoking on pain chronicity, it is imperative that physicians implement strategies to help their patients stop smoking.
Kristoff Kowalkowski- Smarts, skills makes Kowalkowski a success

Smarts, skills make Kowalkowski a success
He would never come out and say it, but when Kristoff Kowalkowski is on the football field he is typically one of the smartest players. Not only is the 11-year-old Duel winner a straight-A student at Madison Elementary School in St. Cloud, Minn., Kowalkowski comes from a football family. Oh yeah, he can also speak and write Chinese thanks to participating in an immersion program at school. It’s little wonder Kowalkowski has a complete understanding of whatever offense he is running. “I like being one of the leaders on the field,” the 5-foot-3, 110-pounder said. “It’s really fun when you learn everything and then you can just see it come together on the field. And I like picking apart defenses.” While he is still developing his game, Kowalkowski has already established himself as a dangerous QB capable of shredding the opposition.
Turnover free
Playing for the St. Cloud/Apollo Mustangs last season, he led his team to a 4-2 record and did not throw an interception or turn the ball over all year. He did have 6 touchdown passes and multiple games with over 100 yards passing. “I think it’s important,” Kowalkowski said. “When you don’t turn the turn the ball over, you’re not going to give the other team chances to score. If there’s a defender within 3 yards of where I want to throw the ball, I’m not going to throw it.” Kowalkowski threw the ball extremely well at the Duel in July, winning NFA’s showcase event in his age group. “I just wanted to go there and do my best and see what happens,” he said. “Finishing in first place, it makes me feel pretty cool. It was a great competition and to do so well, I think I’m pretty confident heading into my season.”
Back with the Mustangs this year, Kowalkowski is looking to build off the success he had in 2013. “Just like last season, I don’t want to turn the ball over,” he said. “And hopefully, we can score more touchdown and make more yards after completions and rush for more yards.”
NFA boost
For the past two years, Kowalkowski has been training with NFA to help sharpen his quarterback skills. It has obviously been paying off. “NFA has helped me with a lot of my mechanics and footwork,” he said. “I want to get better with my footwork. My mechanics are pretty good but with better footwork I’ll be able to move a lot better. I also work a lot with my dad.” Tom Kowalkowski played college football at St. John’s University in Minnesota under legendary Head Coach John Gagliardi, who retired after the 2012 season with a 489-138-11 record, making him the winningest coach in collegiate history. Tom is thrilled his son has hooked up with NFA. “I think it’s a wonderful program,” he said. “It really helps the kids. More importantly, they’re teaching them a philosophy about life, and that’s more important than football. I’ve been very impressed with NFA.”
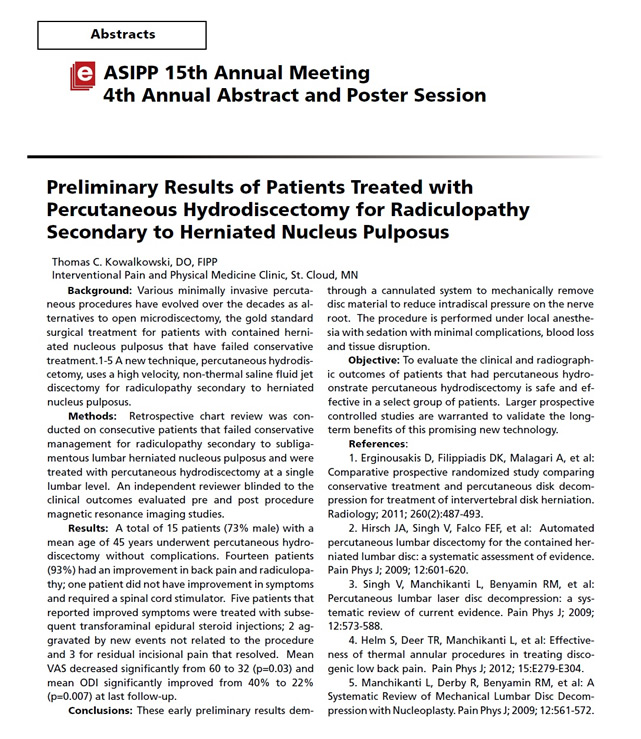
Dr. Thomas Kowalkowski, Medical Director of IPPMC, Intervention Pain and Physical Medicine Clinic, recently was selected to present his research findings, at the Annual Scientific Research meeting in Orlando, Florida. His presentation title was The results of Patients treated with Percutaneous Hydrodiscectomy for Radiculopathy Secondary to Herniated Nucleus Pulposis. The International Spine Interventional Society (ISIS), is an organization of over 3,000 physicians dedicated to the development and promotion for the highest standards of practice of interventional procedures in the diagnosis and treatment of spine pain.
"Water Jet" treatment at Sartell Clinic offers chance to wash away that disc pain

Photo by: Jason Wachter
Dr. Thomas Kowalkowski, medical director of the Interventional Pain and Physical Medicine Clinic in Sartell, shows a new device called HydroCision Sept. 17. The device is a minimally invasive treatment that uses high-speed water to remove herniated disc tissue without invasive surgery.
Who is a good candidate for HydroCision?
- Those with a bulging spinal disc that has not ruptured into the spinal canal.
- Someone whose pain has not improved after four or more weeks of conservative care, which typically consists of physical therapy, pain medications, and if necessary, epidural steroid injections.
- A person with signs of nerve damage in the leg (severe weakness, loss of coordination, loss of feeling).
Source: HydroCision Inc.
After undergoing HydroCision for herniated discs
- In most cases, you will be able to go home the same day as your procedure.
- Plan on bed rest with gentle stretching for several days.
- You may need over-the-counter or prescription pain medication for several days.
Source: HydroCision Inc.
What if you could “wash away” back and leg pain using a “blade” that never gets dull?
A powerful water jet cutting device can be used for minimally invasive treatment of herniated discs, and Dr. Thomas Kowalkowski is the only physician in Central Minnesota to offer the procedure. “It’s basically a high-velocity water jet eroding system,” Kevin Staid said about the medical device that his North Billerica, Mass.-based company makes. “And this is our first entry into the area.”
With HydroCision, a jet of saline solution comes out of a nozzle that is 0.005 inches in diameter — “slightly larger than a hair” — and can cut away protruding disc tissue that can cause the back and leg pain without an actual blade.
“Just the energy of the jet would be doing the cutting,” said Staid, an engineer. “In our case, the water is going about 600 miles an hour and has the ability to cut quite effectively.”
The advantages of the 20-minute outpatient procedure are: No hospitalization, quicker recovery times, less pain, no surgical trauma to the back muscles and no general anesthesia. “There is no muscle damage, no bone removal, no nerve root manipulation ... and the size of the wound is approximately 4 mm,” Kowalkowski said.
Kowalkowski began offering HydroCision a few years ago to his patients; he is the medical director of the Interventional Pain and Physical Medicine Clinic in Sartell.
“The procedure and the study I have completed on it was published in a pain journal this summer,” he said of the official publication of the International Association for the Study of Pain.
HydroCision
Water-based tools previously have been used outside the medical field. “They were used in the aerospace industry and automotive industry for cutting and preparing things ... because the blade never gets dull or gunky,” Staid said.
HydroCision Inc. brought its cutting device into the medical field in 2005, and disc treatment is one of the uses.
When the outer wall of a spinal disc becomes damaged or weakened through age or injury, the inner part of the disc may bulge out in what is known as “disc herniation” or a “slipped” disc.
The water jet comes out of a tiny tube at the end of a spark plug-like tip and is collected — along with the blasted tissue — in another tube built into the same probe, completing a circuit of sorts.
“When the physician’s foot is not on the control pedal, it’s nothing but a benign metal probe,” said Staid, who came up with the concept with Tim Moutafis, a colleague.
Staid is the chief technology officer and vice president of application development at HydroCision Inc., a developer and manufacturer of fluidjet-based surgical tools.
“He (Moutafis) came upon the idea of using high-velocity water jets as a tool, which had been used extensively in industry but not had been developed for use in medicine at all,” Staid said. Kowalkowski said, “I really became intrigued with the technology, to a point that we’ve performed probably over 50 procedures, and many of those patients have been offered surgery as an option for their disc herniation.”
Spinal discs
Only spinal discs that have not ruptured may be treated with the water-based procedure, according to Kowalkowski.
HydroCision costs about $2,000 to perform at his Sartell clinic and may be covered by insurance — compared with the estimated $15,000 it would cost for surgery, he said.
“There is a week’s recovery time versus, many times, eight weeks or more with surgery,” Kowalkowski said.
He also said that in the worst-case scenario that HydroCision does not work, the patient could still have surgery; HydroCision has between a 73 and 98 percent success rate.
The physician uses a fluoroscope, which is a machine that projects live X-ray images onto a monitor, to place the water-dispensing probe within the disc.
“The patient is not even fully anesthetized. They’re awake and alert on the table,” Staid said.
The system has been used in more than 45,000 spinal, arthroscopic and wound debridement procedures, according to HydroCision Inc.
“We’ve been able to document a physiological reduction in the size of the disc immediately after the procedure,” Kowalkowski said
Harnessing physics
Most people in the United States will experience lower back pain at least once during their lives, and more severe leg pain can affect one’s ability to walk, according to the Mayo Clinic.
“At the end of the day, it was hard to even walk because I just ached so bad, and I couldn’t do the activities that I used to be able to do,” said Amy Rasmussen, a patient of Kowalkowski’s.
The 36-year-old registered nurse from Zimmerman said based on her work in a health care setting, she believes not a lot of physicians are aware of HydroCision Inc.
“I work in patient care, and I was lifting a patient and that kind of ruined my back,” Rasmussen said. Her injury occurred when she was working with a 350-pound patient.
She said she has experienced lower back pain, swelling, and achy hips and legs because of the injury and had a lot of frustration before she tried HydroCision in August.
“I figured it was worth it to try this procedure because when you are in that much pain, you’re willing to do anything, and the minute the procedure was done, that pain was gone immediately,” she said.
Source: Stcloudtimes.com
New, Moving or Expanding: IPPMC Welcomes MRI Machine
Practice recently earned excellence award
Source: Stcloudtimes.com

SARTELL — A 5,000-square-foot expansion is nearing completion at the Interventional Pain & Physical Medicine Clinic (IPPMC). One of the latest pieces to fall in place was a new 12,000-pound MRI machine workers moved into place Monday with a forklift.
IPPMC started in 2003 in a small building on Stearns Way. Five years later, it moved to a 15,000-square-foot building at 2301 Connecticut Ave. The additional 5,000 feet was necessary to accommodate more patients and staff, according to Dr. Thomas Kowalkowski, who founded the practice.
For three years, the clinic had been using an MRI machine in a semi trailer parked outside the front door.
“This is a newer machine, and it’s going to be a permanent part of our facility, so we can continue to provide people the best care possible,” said Kowalkowski, who graduated from St. John’s University, the University of New England and completed a fellowship in anesthesiology and pain medicine at Oregon Health and Science University.
IPPMC has about 50 employees, and its building now features everything from an organic coffee and juice bar to a whirlpool, exercise pool and sauna, to a fully-stocked gym. The clinic also has openings for nine more full- and part-time positions.
“I wanted to come back here because this is home to me,” Kowalkowski said. “We’re the only multidisciplinary pain program of this level outside the Twin Cities, and people are responding to that.”
Earlier this month, IPPMC earned the Excellence in Pain Practice Award from the World Institute of Pain.
IPPMC is one of 17 pain centers in 11 countries to receive the honor.
WIP announces Excellence in Pain Practice Award recipient
WINSTON-SALEM, North Carolina, USA (March 11, 2013) – The World Institute of Pain (WIP) has conferred the Excellence in Pain Practice (EPP) Award for Multidisciplinary Clinical Pain Practice on the Interventional Pain and Physical Medicine Clinic (IPPMC) in Sartell, Minnesota, USA.
“IPPMC’s attributes include providing a multidisciplinary pain centered approach to the prevention, evaluation, treatment, and rehabilitation of painful disorders,” said Dr. Bruce Wymore, a family practitioner in Alexandria, Minnesota.
Dr. Jose Veliz, a pain medicine specialist in Escondido, California added that IPPMC Medical Director Dr. Thomas Kowalkowski has, “a true passion for pain medicine.“
In conveying the award, WIP’s EPP Award Committee Chairman, Dr. P. Prithvi Raj said, “The Committee found the Interventional Pain and Physical Medicine Clinic’s multidisciplinary approach to clinical pain practice to be exemplary. The impact of this pain center on the specialty of pain practice is evident through its individualized approach to improving the quality of life by reducing pain and suffering, through teamwork and a multi-disciplinary model of care.”
The EPP Award program, established in 2010 by the World Institute of Pain, recognizes pain centers that demonstrate the highest standards of pain practice around the world. Varying levels of recognition are attainable, including specialization in a particular area of clinical pain practice, multidisciplinary clinical pain practice, and comprehensive recognition that encompasses all dimensions of pain management including cutting-edge research. EPP Awards have been conferred on 17 pain centers in 11 countries.
To qualify for the award, a site visit is conducted by an FIPP (Fellow of Interventional Pain Practice) member of WIP’s inspector’s panel. The EPP Award Committee exercises its due diligence in the determination of each award given, in accordance with WIP’s guidelines for EPP Award recognition.
WIP is an international, nonprofit organization founded in 1993 that brings together the most recognized experts in the field of pain medicine for the advancement and standardization of interventional pain practice. WIP achieves its purposes and objectives through organizing physician-oriented educational symposia, practical workshops, and World Congresses; certifying as Fellows of Interventional Pain Practice (FIPP) physicians who pass a competency-based, multi-part examination; publishing the scholarly journal, Pain Practice; and establishing liaisons with physicians and industry worldwide to promote the specialty of pain medicine.
IPPMC Patients need NOT be concerned with the multi-state meningitis and septic arthritis outbreak.
IPPMC has not utilized these pharmaceutical products. All medications at IPPMC are FDA Approved. IPPMC is dedicated to offering the highest standard of care based on patient outcomes.
- The CDC continues to update the public with information on the current case count, case definitions, testing and diagnostic recommendations, and treatment guidance among other items. Please check the CDC website daily for ongoing updates and new information on this outbreak: http://www.cdc.gov/hai/outbreaks/meningitis.html
- CDC and FDA have confirmed the presence of a fungus known as Exserohilum rostratum3in unopened medication vials of preservative-free methylprednisolone acetate (80mg/ml) from one of the three implicated lots from NECC (Lot #08102012@51, BUD 2/6/2013). The laboratory confirmation further links steroid injections from these lots from NECC to the multistate outbreak of fungal meningitis and joint infections. Testing on the other two implicated lots of methylprednisolone acetate and other NECC injectables continues.
- CDC and state health departments estimate that approximately 14,000 patients may have received injections with medication from three implicated lots of methylprednisolone and nearly 97% of these patients have been contacted for further follow-up.
- Clinicians are also requested to report any suspected adverse events following use of these products to FDA's MedWatch program at 1-800-332-1088 or www.fda.gov/medwatch4.
- Health care professionals and patients may dial FDA’s Drug Information Line at 855-543-DRUG (3784) and press * to get the most recent information regarding the meningitis recall and speak directly to a pharmacist.
- There is now available a Patient Notification Letter5 on the FDA "Update on Fungal Meningitis" webpage under the "Related Information" section. This letter template is for healthcare professionals notifying patients administered a drug produced by the New England Compounding Center (NECC) that has been recalled.
FDA released an updated statement on the fungal meningitis outbreak:http://www.fda.gov/Drugs/DrugSafety/ucm322734.ht
Ginkgo Biloba: No-Go for Alzheimer's Prevention
Another large trial shows no benefit from ginkgo biloba extract in preventing Alzheimer disease, researchers report in the Lancet Neurology.
Nearly 2900 older adults without dementia who spontaneously reported memory complaints to their physicians were randomized to consume standardized ginkgo biloba extract or placebo for 5 years. Overall, the rate of diagnosis with probable Alzheimer's did not differ significantly between the ginkgo and placebo groups (1.2 and 1.4 cases per 100 person-years).
The authors note that a lower-than-expected Alzheimer's rate in both groups reduced the study's power, while a Lancet Neurology editorialist concludes: "For adults aged 70 years or older with a memory complaint who might be mildly cognitively impaired, use of [ginkgo biloba extract] does not decrease the risk of Alzheimer's disease over 5 years."
New Way of Fighting High Cholesterol Upends Assumptions
Atherosclerosis – the hardening of arteries that is a primary cause of cardiovascular disease and death – has long been presumed to be the fateful consequence of complicated interactions between overabundant cholesterol and resulting inflammation in the heart and blood vessels.
However, researchers at the University of California, San Diego School of Medicine, with colleagues at institutions across the country, say the relationship is not exactly what it appears, and that a precursor to cholesterol actually suppresses inflammatory response genes. This precursor molecule could provide a new target for drugs designed to treat atherosclerosis, which kills tens of thousands of Americans annually.
The findings are published in the September 28, 2012 issue of Cell.
Lurking within our arterial walls are immune system cells called macrophages (Greek for “big eater”) whose essential function is to consume other cells or matter identified as foreign or dangerous. “When they do that, it means they consume the other cell’s store of cholesterol,” said Christopher Glass, MD, PhD, a professor in the Departments of Medicine and Cellular and Molecular Medicine and senior author of the Cell study. “As a result, they’ve developed very effective ways to metabolize the excess cholesterol and get rid of it.”
But some macrophages fail to properly dispose of the excess cholesterol, allowing it to instead accumulate inside them as foamy lipid (fat) droplets, which gives the cells their particular name: macrophage foam cells.
These foam macrophages produce molecules that summon other immune cells and release molecules, signaling certain genes to launch an inflammatory response. Glass said conventional wisdom has long assumed atherosclerotic lesions – clumps of fat-laden foam cells massed within arterial walls – were the unhealthy consequence of an escalating association between unregulated cholesterol accumulation and inflammation.
Glass and colleagues wanted to know exactly how cholesterol accumulation led to inflammation, and why the macrophages failed to do their job. Using specialized mouse models that produced abundant macrophage foam cells, they made two unexpected discoveries that upend previous assumptions about how lesions form and how atherosclerosis might be more effectively treated.
“The first is that foam cell formation suppressed activation of genes that promote inflammation. That’s exactly the opposite of what we thought happened,” said Glass. “Second, we identified a molecule that helps normal macrophages manage cholesterol balance. When it’s in abundance, it turns on cellular pathways to get rid of cholesterol and turns off pathways for producing more cholesterol.”
That molecule is desmosterol – the final precursor in the production of cholesterol, which cells make and use as a structural component of their membranes. In atherosclerotic lesions, Glass said the normal function of desmosterol appears to be “crippled.”
“That’s the next thing to study; why that happens,” Glass said, hypothesizing that the cause may be linked to overwhelming, pro-inflammatory signals coming from proteins called Toll-like receptors on macrophages and other cells that, like macrophages, are critical elements of the immune system.
The identification of desmosterol’s ability to reduce macrophage cholesterol presents researchers and drug developers with a potential new target for reducing the risk of atherosclerosis.
Glass noted that a synthetic molecule similar to desmosterol already exists, offering an immediate test-case for new studies. In addition, scientists in the 1950s developed a drug called triparanol that inhibited cholesterol production, effectively boosting desmosterol levels. The drug was sold as a heart disease medication, but later discovered to cause severe side effects, including blindness from an unusual form of cataracts. It was pulled from the market and abandoned.
“We’ve learned a lot in 50 years,” said Glass. “Maybe there’s a way now to create a new drug that mimics the cholesterol inhibition without the side effects.”
Co-authors are first author Nathanael J. Spann, Norihito Shibata, Donna Reichart, Jesse N. Fox and Daniel Heudobler, UCSD Department of Cellular and Molecular Medicine; Lana X. Garmire, UCSD Department of Bioengineering; Jeffrey G. McDonald and David W. Russell, Department of Molecular Genetics, UT Southwestern Medical Center; David S. Myers, Stephen B. Milne and Alex Brown, Department of Pharmacology, Vanderbilt Institute of Chemical Biology; Iftach Shaked and Klaus Ley, La Jolla Institute of Allergy and Immunology; Christian R.H. Raetz, Department of Biochemistry, Duke University School of Medicine; Elaine W. Wang, Samuel L. Kelly, M. Cameron Sullards and Alfred H. Merrill, Jr., Schools of Biology, Chemistry and Biochemistry and the Parker H. Petit Institute of Bioengineering and Bioscience, George Institute of Technology; Edward A. Dennis, UCSD Department of Chemistry and Biochemistry; Andrew C. Li, Sotirios Tsimikas and Oswald Quehenberger, UCSD Department of Medicine; Eoin Fahy, UCSD Department of Bioengineering; and Shankar Subramaniam, UCSD Departments of Cellular and Molecular Medicine, Bioengineering and Chemistry and Biochemistry.
Funding for this research came, in part, from National Institutes of Health grants GM U54069338 (to the LIPID MAPS Consortium), P01 HC088093 and P01 DK074868.
Source: health.ucsd.edu
FDA Introduces New Safety Measures for Extended-Release & Long-acting Opioid Medications
The U.S. Food and Drug Administration today approved a risk evaluation and mitigation strategy (REMS) for extended-release (ER) and long-acting (LA) opioids, highly potent drugs approved for moderate to severe, persistent pain that requires treatment for an extended period.
The REMS is part of a federal initiative to address the prescription drug abuse, misuse, and overdose epidemic. The REMS introduces new safety measures designed to reduce risks and improve the safe use of ER/LA opioids, while ensuring access to needed medications for patients in pain.
"Misprescribing, misuse, and abuse of extended-release and long-acting opioids are a critical and growing public health challenge,” said FDA Commissioner Margaret A. Hamburg, M.D. "The FDA’s goal with this REMS approval is to ensure that health care professionals are educated on how to safely prescribe opioids and that patients know how to safely use these drugs.”
The new ER/LA opioid REMS will affect more than 20 companies that manufacture these opioid analgesics. Under the new REMS, companies will be required to make education programs available to prescribers based on an FDA Blueprint. It is expected that companies will meet this obligation by providing educational grants to continuing education (CE) providers, who will develop and deliver the training.
The REMS also will require companies to make available FDA-approved patient education materials on the safe use of these drugs. The companies will be required to perform periodic assessments of the implementation of the REMS and the success of the program in meeting its goals. The FDA will review these assessments and may require additional elements to achieve the goals of the program.
"We commend the FDA for taking action to save lives by increasing access to prescriber education,” said Gil Kerlikowske, director of the Office of National Drug Control Policy. "Since day one, the Obama Administration has been laser focused on addressing the prescription drug abuse epidemic and today’s action is an important contribution to this comprehensive effort.”
ER/LA opioid analgesics are widely prescribed medicines with an estimated 22.9 million prescriptions dispensed in 2011, according to IMS Health, which provides services and information to the health care and pharmaceutical industries. It is estimated that more than 320,000 prescribers registered with the Drug Enforcement Administration (DEA) wrote at least one prescription for these drugs in 2011.
ER/LA opioid analgesics are associated with serious risks of overuse, abuse, misuse and death and the numbers continue to rise. According to the Centers for Disease Control and Prevention, 14,800 Americans died from overdoses involving opioids in 2008. In 2009, there were 15,597 deaths involving these medications – nearly four times as many deaths compared to 1999.
"Misuse and abuse of prescription opioids is a complex problem and demands a holistic response,” said John Jenkins, M.D., director of CDER’s Office of New Drugs. "The new REMS program is one component of a multi-agency, national strategy to address this important public health issue.”
Key components of the ER/LA opioid analgesics REMS include:
Training for prescribers
Based on an FDA Blueprint, developed with input from stakeholders, educational programs for prescribers of ER/LA opioids will include information on weighing the risks and benefits of opioid therapy, choosing patients appropriately, managing and monitoring patients, and counseling patients on the safe use of these drugs. In addition, the education will include information on how to recognize evidence of, and the potential for, opioid misuse, abuse, and addiction, and general and specific drug information for ER/LA opioid analgesics.
Updated Medication Guide and patient counseling document
These materials contain consumer-friendly information on the safe use, storage and disposal of ER/ LA opioid analgesics. Included are instructions to consult one’s physician or other prescribing health care professional before changing doses; signs of potential overdose and emergency contact instructions; and specific advice on safe storage to prevent accidental exposure to family members and household visitors.
Assessment/auditing
Companies will be expected to achieve certain FDA-established goals for the percentage of prescribers of ER/ LA opioids who complete the training, as well as assess prescribers’ understanding of important risk information over time. The assessments also cover whether the REMS is adversely affecting patient access to necessary pain medications, which manufacturers must report to FDA as part of periodic required assessments.
It is expected that the first continuing education activities under the REMS will be offered to prescribers by March 1, 2013.
There is no mandatory requirement that prescribers take the training and no precondition to prescribing ER/LA opioids to patients. However, the Obama Administration endorsed a mandatory training program on responsible opioid prescribing practices in April 2011 as part of its comprehensive plan to address the epidemic of prescription drug abuse. The program, which would be linked to DEA registration by providers, would require legislative changes that are being pursued by the Administration.
The FDA continues to support this approach, but absent the needed legislation, intends to exercise its authority to require mandatory elements for companies and voluntary elements for prescribers – all of which are important and necessary steps to help curb the misuse and abuse of ER/ LA opioid analgesics, without being overly burdensome.
Source: Spinalinjection.org
New Back Pain Gene Identified
Researchers at King’s College London have for the first time identified a gene linked to age-related degeneration of the intervertebral discs in the spine, a common cause of lower back pain.
Costing the UK an estimated £7billion a year due to sickness leave and treatment costs, the causes of back pain are not yet fully understood. Until now, the genetic cause of lower back pain associated with lumbar disc degeneration (LDD) was unknown, but the largest study to date, published this week in the journal Annals of Rheumatic Diseases, has revealed an association with the PARK2 gene.
The researchers, funded by the Wellcome Trust and Arthritis Research UK, say more research into this surprising association needs to be carried out in order to fully understand how it is triggered, but this new finding could ultimately pave the way towards developing new treatments in the future.
LDD is a common age-related trait, with over a third of middle-aged women having at least one degenerate disc in the spine. Discs become dehydrated, lose height and the vertebrae next to the discs develop bony growths called osteophytes. These changes can cause or contribute to lower back pain. LDD is inherited in between 65 – 80 per cent of people with the condition, suggesting that genes play a key role.
Scientists compared MRI images of the spine in 4,600 individuals with genome-wide association data, which mapped the genes of all the volunteers. They identified that the gene PARK2 was implicated in people with degenerate discs and could affect the speed at which they deteriorate.
The researchers say the results show that the gene may be switched off in people with LDD. Although it is still unclear how this might happen, it is thought that environmental factors, such as lifestyle and diet, could trigger this switch by making changes known as epigenetic modifications to the gene.
Dr Frances Williams, Senior Lecturer from the Department of Twin Research and Genetic Epidemiology at King’s College London, said: 'Back pain can have a serious impact on people’s lives and is one of the most common causes of sickness leave, costing both the NHS and UK economy billions each year.
'We have performed, using data collected from around the world, the biggest genome-wide association analysis of lumbar disc degeneration (LDD). We know that people whose discs wear out are at increased risk of episodes of lower back pain, but normal human discs are hard to get hold of to study so until now our knowledge of normal human biology was incomplete.
'We have identified a gene called PARK2 as associated with LDD. We have shown that the gene may be switched off in people with the condition.
'Further work by disc researchers to define the role of this gene will, we hope, shed light on one of most important causes of lower back pain. It is feasible that if we can build on this finding and improve our knowledge of the condition, we may one day be able to develop new, more effective treatments for back pain caused by this common condition.'
Source: ScienceDaily
IPPMC Earns ACR Accreditation

Interventional Pain & Physical Medicine Clinic has been awarded a three-year term of accreditation in magnetic resonance imaging (MRI) as the result of a recent review by the American College of Radiology (ACR). MRI is a noninvasive medical test that utilizes magnetic fields to produce anatomical images of internal body parts to help physicians diagnose and treat medical conditions.
The ACR gold seal of accreditation represents the highest level of image quality and patient safety. It is awarded only to facilities meeting ACR Practice Guidelines and Technical Standards after a peer-review evaluation by board-certified physicians and medical physicists who are experts in the field. Image quality, personnel qualifications, adequacy of facility equipment, quality control procedures, and quality assurance programs are assessed. The findings are reported to the ACR Committee on Accreditation, which subsequently provides the practice with a comprehensive report they can use for continuous practice improvement.
The ACR is a national professional organization serving more than 34,000 diagnostic/interventional radiologists, radiation oncologists, nuclear medicine physicians, and medical physicists with programs focusing on the practice of medical imaging and radiation oncology and the delivery of comprehensive health care services.
Thomas Kowalkowski
Fellow of ABPM&R, DO,FIPP Medical Director

Board Certified
American Board of Physical Medicine and Rehabilitation
Subspecialty of Pain Medicine
World Institute of Pain
Diplomate of the American Board of Interventional Pain Physicians
Residency
Physical Medicine & Rehabilitation, University of Minnesota
Medical Education
University of New England (COM)
Undergraduate: St. John's University, Collegeville, MN
Fellowship: ACGME Fellowship in Anesthesiology/Pain medicine, Oregon Health and Science University
Dr. Kowalkowski practices Interventional Pain and Sports medicine full time. He is a diplomate of the American Board of Physical Medicine and Rehabilitation from the University of Minnesota with a sub-specialty in pain medicine. He has completed an ACGME Fellowship in Anesthesiology/Pain Medicine from Oregon Health and Science University. Dr. Kowalkowski is a Fellow of Interventional Pain Practice (FIPP), the only certifying agency which tests the ability to perform interventional pain procedures. He is a member of the American Society of Anesthesiologists, The World Institute of Pain, American Society of Interventional Pain Physicians, North American Spine Society, International Spinal Injection Society, and PASSOR (Physiatrist Association of Spine, Sport, and Occupational Rehabilitation).
Dr. Kowalkowski is one of less than 100 physicians across the country with his specific training and credentials in pain medicine. He is dedicated to the diagnosis of acute and chronic pain conditions of complex musculoskeletal, orthopedic, and neurological problems pertaining to pain medicine. Dr. Kowalkowski is committed to providing you with the best possible care using an individualized approach. The practice focuses on interventional pain medicine using state of the art technology in the treatment of pain